Prolapse is Confusing!
If you've been diagnosed with, or ever suspected that you have, pelvic organ prolapse, I'm certain it brings up a million questions for you. Will my bladder eventually fall out of my vagina? Will having sex make it worse? Do I need surgery? What about having more kids, returning to exercise and running, etc etc??
These are all FANTASTIC questions that typically don't get explained very well by the person who diagnoses you with prolapse, or by doing your own internet research. And, most of these difficulties originate with the fact that prolapse is not just one diagnosis. There are so many different organs that can prolapse, and so many different grades of prolapse, that it can be incredibly confusing. So today, let's start with the basics: what is prolapse, and how do we diagnose and grade it?
What is Prolapse?
The definition of prolapse is when "an organ or organs in the pelvic cavity shift downward out of their normal position." (Palm 2017)
What are the Types of Prolapse?
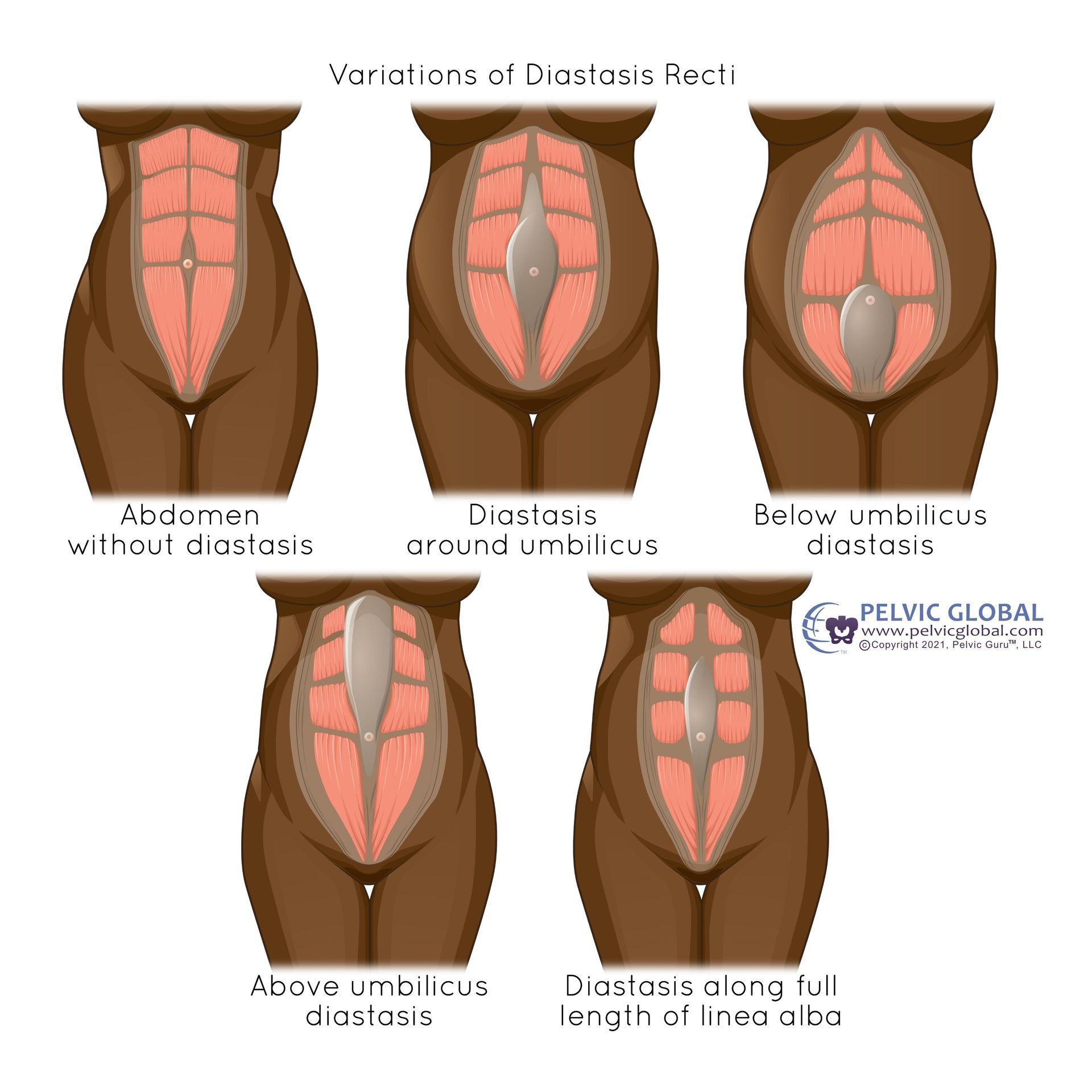
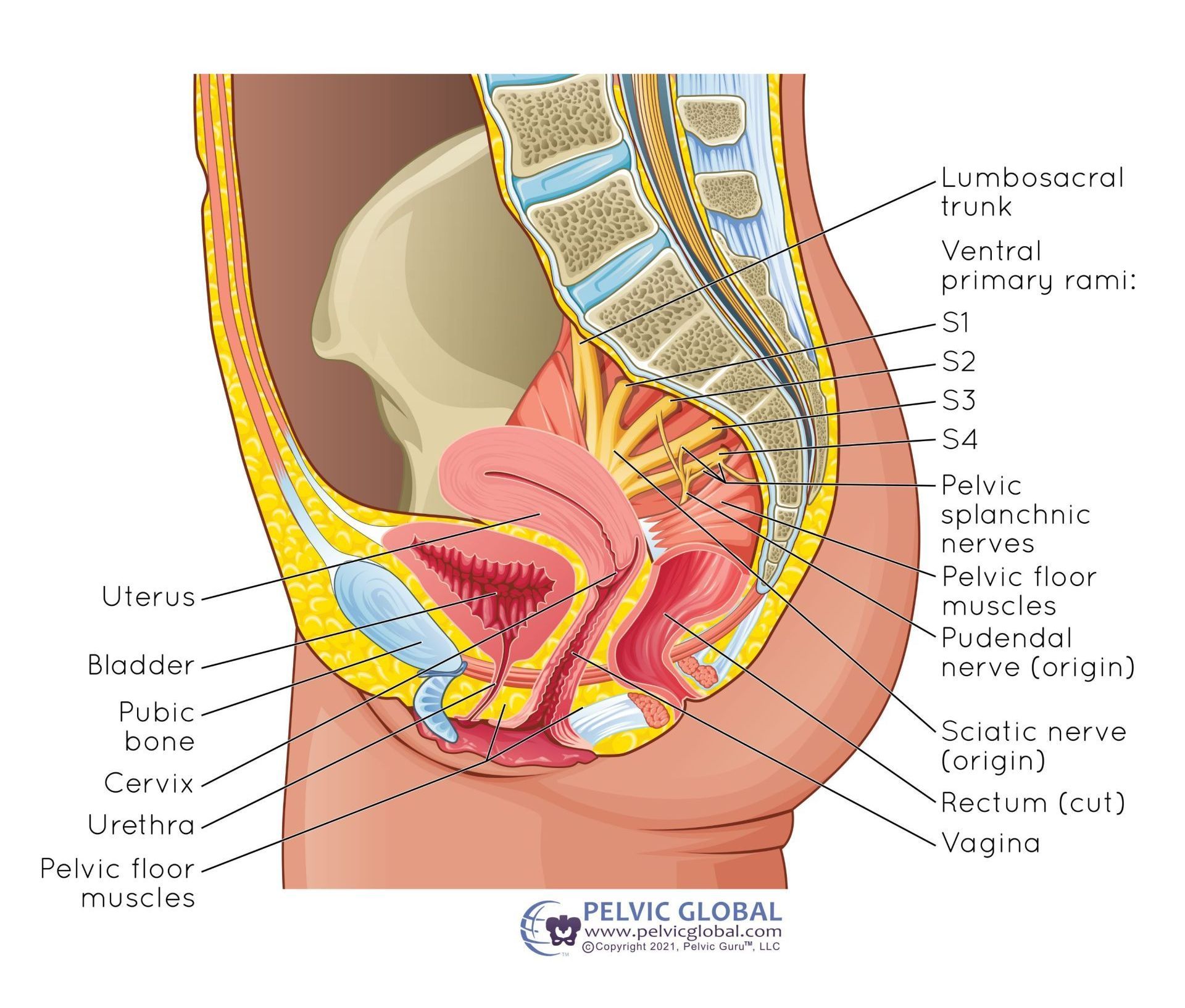
Vaginal prolapse can occur from the bladder (cystocele), the rectum (rectocele), the uterus/cervix (apical or uterine prolapse), the small intestines (enterocele), or the vaginal vault (vaginal vault prolapse only happens in individuals who have had a total hysterectomy).
It's also important to note that similar to a hernia, the “bulge” created by a prolapse is the organ pushing the vaginal wall downwards or outwards. As a result, the tissue you are actually seeing or feeling is the vaginal wall, not the organ itself. So no, your bladder or bowel will not just fall out one day! The only exception to this is cervical/uterine prolapse, where you will actually feel or see the cervix if it gets low enough. But, I promise that still won’t fall out one day either!
You can also have prolapse outside of the vaginal canal - the urethra can descend from its original position towards the vulva (urethrocele), or the lining of the rectum can prolapse outside of the anus (rectal prolapse). {NOTE: this is why language is important; many people will talk about a "rectal prolapse" when they really mean a rectocele. Rectal prolapse external to the anus requires surgical correction - no amount of pelvic floor exercises will help.}
WHEW that's a lot. So, before you freak out and worry about just exactly how many of your organs will eventually fall out of your vagina (haha), let's talk about grading and statistics!
How do we Grade Prolapse?
This is super important. - not all prolapses are created equal! There is a VERY big difference between minor prolapses (the bladder just slightly bulging into the vagina) vs major prolapses (the cervix or uterus being external to the vagina).
There are a few different grading scales out there, but here are the most common grades:
- Prolapse is less than halfway to the opening of the vagina
- Prolapse is more than halfway to, or AT the opening of the vagina
- Prolapse is EXTERNAL TO the opening of the vagina
- Maximal descent of the entire organ outside of the vagina
The good news is that prolapse is a slowly progressing condition. So no, you won't go from a grade 1 to a grade 3 overnight. Grade 4 students are rare, especially in higher-income countries. Typically it takes years for prolapse to worsen, if it does worsen at all. In upcoming posts we'll talk about what does and doesn't cause prolapse, and if you do have prolapse what you can do to help it get better (or at least not get worse).
Who Can Diagnose Me with Prolapse?
This is also an excellent question with a very nuanced answer. Your gynecologist (GYN) can do so, but the prolapse specialists are truly urogynecologists (urogyns) or in some cases colorectal surgeons, particularly for rectoceles. A pelvic floor PT can also diagnose you with prolapse, but we can't say with certainty which organ is prolapsing - we typically talk more about which wall of the vaginal canal is bulging. A pelvic floor PT also typically can do a more detailed assessment than your GYN, as we also can assess people in standing positions. Sometimes prolapses are tricky to see when you are laying flat on your back, so a standing examination can be very useful!
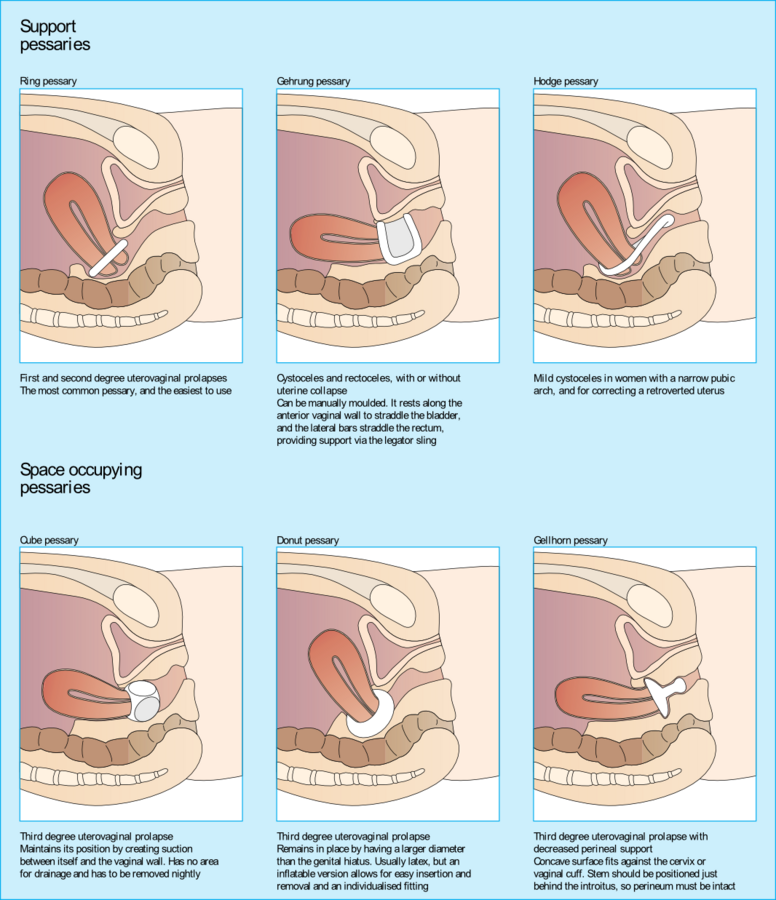
If someone is concerned about their prolapse diagnosis, I do typically recommend they seek a consultation with a urogynecologist. This usually occurs when they have been told they don't have a prolapse when they think they do, or have been blindsided with a diagnosis of higher-degree or multiple-organ prolapse when they were unaware. A urogyn can do a much more detailed assessment of prolapse than a GYN can, and they are also experts at fitting pessaries or performing corrective surgeries. More on this in upcoming posts! But if you are curious, you can look up a urogyn close to you or a colorectalsurgeon (for rectoceles or rectal prolapse).
I will say also that typically fancy imaging studies are not needed to diagnose prolapse. They can be used in certain cases, for example, if you have constipation and a rectocele, there is a special test that can be done to see how much of your rectum is falling into the vagina when you are bearing down to pass stool. But, this is definitely the exception rather than the rule. Usually, the examination done in the office is all that is needed.
What Else Should I Know About Pelvic Organ Prolapse?
Voices for Pelvic Floor Dysfunction
Association for Pelvic Organ Prolapse Support
International Urogynecological Association patient information leaflets
American Urogynecological Association patient fact sheets
Reference:
Palm, S. (2017). Pelvic Organ Prolapse: The Silent Epidemic (3rd ed.). POP Publishing and Distribution.




All Rights Reserved | Pelvic Love Physiotherapy & Wellness, PLLC