KNOWLEDGE CENTER
Knowledge Center

By Jam Rohr
•
January 20, 2025
Prolapse Surgeries, Part II This article is a follow-up to a Part I article I wrote on prolapse surgeries, where I covered a lot of FAQs about who needs surgery and why. In this article, we'll cover the nitty gritty of surgeries, including the different types of surgeries and recovery times, etc. We won't rehash what I mentioned last time, so if you have questions about who might need surgery, and how successful surgery generally is or isn't, please revisit the past article! What types of prolapse surgeries are there? There are two types of surgeries. For most people who are patients at Pelvic Love and who are reading this article, they will have a type of surgery that preserves the ability to have vaginal intercourse. There is another type of surgery that closes off the vagina, but then of course after that, you are no longer able to have intercourse. So that is typically reserved for elderly people with vaginas, as this type of surgery has the highest cure rate for prolapse. But of the types of surgeries that leave the vaginal canal open, there are many options depending upon the type of prolapse. Does surgery vary based on the type of prolapse? Yes! For bladder prolapse, the most common type of surgery is called anterior colporrhaphy . In this procedure, the front wall of the vagina underneath the bladder has sutures placed in it to help reinforce the original position of the bladder. For rectocele (rectal prolapse into the vagina), the most common type of surgery is a posterior colporrhaphy . This also involves placing sutures on the backside of the vaginal wall to help keep the rectum in place. Sometimes this is also done in combination with a repair of the perineal body (the area between the vagina and anus), aka perineorrhaphy. What about uterine/cervical prolapse? This gets a little tricky. Many times, if you are done having children and your prolapse is more advanced, you may be advised to have a hysterectomy . However, there are other options that will allow you to keep your uterus. These surgeries are a little more complicated to explain, but if you click this link , you'll find them explained well. Basically they all involve some method of re-suspending the uterus and the cervix by using either stitches or mesh (NOT the mesh that is involved in so many lawsuits!). If you do opt to have a hysterectomy, then as you may imagine, this can place you at a higher risk of bladder and/or bowel prolapsing (if they have not already done so). The uterus takes up a fair amount of space inside the pelvis, so if you remove it, that leaves empty space for other organs to fall into. If I do have a hysterectomy, what are my options to avoid future issues with prolapse? This is the one topic for which I will drag out my soapbox. If you do have a hysterectomy, and it is an option for you, I would HIGHLY recommend your surgeon re-suspends the vaginal vault as part of your surgery . The vaginal vault is the apex of the vagina, and where the vagina is sewn shut after the uterus/cervix is removed. Many surgeons will just stop here and allow the top of the vagina to essentially scar in place. However, as you can imagine, when you remove a major internal organ, then you are also removing (or slackening) a lot of ligaments & fascia that support that organ and others! So this places the top of the vagina at a much higher risk from prolapsing in the future, and/or the bladder and bowel falling into the vagina. Please note, these "extra" steps to support the top of the vagina during a hysterectomy are not available to everyone . They do require more time under anesthesia, potentially greater skill from your surgeon, and the structures the vaginal vault is being sutured to are still intact. For example, I had a friend that had severe endometriosis and had a hysterectomy at 40 years old as a result. Her endometriosis was so advanced, and so many lesions had to be removed from inside the pelvis, that this didn't leave her surgeon with an option for a good place to suspend her vaginal vault. So even though I would recommend you discuss this with your surgeon, it's not an option for everyone. What are the options for suspending the vaginal vault after hysterectomy? There are many places from which the vaginal vault can be suspended after the uterus/cervix are removed. There are too many to go into detail in this format, but all have their pluses and minuses. The main options are the uterosacral ligament , sacrospinous ligament , and the sacrum itself . More general information can be found in this handout . What is recovery like after these types of surgeries? Every surgeon is different, but here are some general guidelines for recovering from a hysterectomy or prolapse repair. And YES, many times there is more than one repair being done at a time! Or a hysterectomy may be combined with an anterior and/or posterior vaginal wall repair, for example. Most often, you will have a catheter in place for anywhere from 8-24 hours after surgery (potentially longer for a bladder repair). And generally, your hospital stay is very short. Typically you need to take anywhere from 2-6 weeks off work. Around 2-3 weeks you can resume driving and taking short walks. And no sex (vaginal penetration) is allowed for 6 weeks. It's also important to remember that because these are very delicate tissues, they are not fully healed for THREE MONTHS. So, for quite some time you will likely have restrictions on heavy lifting. Have even more questions about your pelvic floor in general, or prolapse specifically? Here are two great websites for more info on all kinds of pelvic floor-related issues, not just prolapse: International Urogynecological Association handouts American Urogynecologic Society fact sheets References: All information contained in this post is aggregated from the handouts linked throughout the text.

By Jam Rohr
•
January 20, 2025
Prolapse Surgeries, Part I Whew, surgery for prolapse is a big topic. So much so that I'm splitting it into two articles to avoid overloading your eyeballs and brains! Today we'll spend time discussing the whys and who's surrounding surgery. Then next time we'll get into the details of types of surgeries, recovery times, etc. If I have prolapse, do I definitely need surgery? In a word, no. Or at least, most likely not. I wanted to get this question out of the way first, because I think prolapse can be a very scary diagnosis when you are first told you have it. Then, your brain (or at least mine!) jumps to the most extreme outcome, which would be surgery. As we discussed in a past article about the best exercises for prolapse, pelvic floor muscle training and core strengthening can be a really effective treatment for prolapse. It can relieve your symptoms, delay/prevent the need for surgery, and potentially even reduce the grade of your prolapse. Plus, pessaries are another great non-surgical option that can prevent or delay the need for surgery too (if the idea of a pessary is new to you, check out my past article on pessaries). So, especially if you are newly diagnosed with prolapse, don't jump to the thought that you will have to have surgery someday! Who does need surgery for prolapse? Indications for prolapse surgery are the following: Significant "bother" of symptoms (vaginal heaviness/pressure, associated bowel/bladder symptoms, difficulty/pain with intercourse, etc) "Failed" a good trial of conservative treatment - PT/pelvic floor muscle training, pessaries, etc. that does not satisfactorily resolve symptoms Completed childbearing Typically more-advanced prolapse grades (3-4), unless with lesser grades the symptoms are severe and not responding to conservative treatment If your prolapse is mild (grade 1-2), you are going to have more children, or have other medical conditions that would make surgery difficult, then you can/should avoid it! Typically the biggest differentiator regarding the need for surgery is if the prolapse extends beyond the hymen, or external to the vagina. Conservative treatment is less likely to be successful (but not always, of course!) in cases where the prolapse is external to the vaginal opening. More often than not, surgery will eventually be needed to resolve symptoms. But, that doesn’t mean a good trial of conservative treatment isn’t a good idea! How common is prolapse surgery? It is pretty common, at least with age. If you have a uterus/vagina, you have a lifetime risk of 11-20% of undergoing surgery for prolapse or stress incontinence. By age 80 the risk is 20%. How successful is prolapse surgery? It is very successful, especially in the short term! Success rates are generally around 80-90%, especially within the first 2 years following surgery. However, it is true generally that the further away you get from surgery, the more likely your prolapse may return. And we don't have a lot of high-quality studies that follow people after prolapse surgeries beyond 2 years (many stop around 6-12 months). The other caveat here is how we define "success." There is a BIG difference between restoring your anatomy (i.e., reducing the organ back to its original position, and having it stay there) and improving your symptoms. Around 5 years post-op, the majority of repairs will have "failed" in terms of anatomy. Meaning that if someone did a vaginal examination, the prolapse will have returned (although potentially not to the same degree that it was present before). However, even in these cases, the symptoms are still reported to be much better, and happiness with surgery outcomes is still high. So this is further proof that the degree of prolapse isn’t always equal to the severity of symptoms and that more research is definitely needed. Why do prolapse surgeries fail? There are a lot of reasons. The biggest one is that the tissues surgeons are trying to repair are very delicate. There's a really fine line between suspending an organ via it's own ligaments, or using mesh, with just enough tension vs. using too much tension. So it's always a balance between fixing the original problem without causing further complications. The other is that many times, the original cause of the prolapse has not been corrected. As I discussed at length in my intra-abdominal pressure article, prolapse really is a top-down problem more than a bottom-up problem. In fact, one recent study that looked at outcomes 5 years after prolapse surgery found no difference between those who did and did not do post-operative pelvic floor muscle training (Jelovsek 2018). Essentially, pelvic floor muscle training did not stop the prolapse from returning. So if you still are doing a lot of heavy lifting, have continued constipation, or are just genetically predisposed to having prolapse, there is a high likelihood it will return because there is still a lot of top-down pressure on your internal organs. It's important to note though, as I stated above, generally, your symptoms still remain improved even if the prolapse itself returns post-operatively. Although of course, some people will need to have a second surgery. This is also why it's best to delay surgery for as long as possible. Should I have prolapse surgery? This is obviously a very personal decision, and depends upon a lot of factors! I think the biggest takeaways here are that you should try PT, pelvic floor & core exercises, and/or pessaries first. Pelvic Love also fits in well with these exercise recommendations, and has some specific videos for prolapse! All of these things are recommended to be the first-line interventions for prolapse and can help the majority of people who are living with prolapse. If that doesn't work for you, or for whatever reason your surgeon determines surgery is the best route right away, then definitely consider it. It can be very successful, especially for symptom improvement! As with any surgery though, I would always recommend getting at least 2 opinions before deciding to move forward. And I would highly recommend at least one of those opinions come from a urogynecologist or colorectal surgeon depending upon your needs. The next article will discuss different options for prolapse surgeries, so be sure to check that one out! References: Bureau, M., & Carlson, K. V. (2017). Pelvic organ prolapse: A primer for urologists. Canadian Urological Association journal = Journal de l'Association des urologues du Canada , 11 (6Suppl2), S125–S130. https://doi.org/10.5489/cuaj.4634 Dumoulin, C., Hunter, K. F., Moore, K., Bradley, C. S., Burgio, K. L., Hagen, S., Imamura, M., Thakar, R., Williams, K., & Chambers, T. (2016). Conservative management for female urinary incontinence and pelvic organ prolapse review 2013: Summary of the 5th International Consultation on Incontinence. Neurourology and urodynamics , 35 (1), 15–20. https://doi.org/10.1002/nau.22677 Jelovsek, J. E., Barber, M. D., Brubaker, L., Norton, P., Gantz, M., Richter, H. E., Weidner, A., Menefee, S., Schaffer, J., Pugh, N., Meikle, S., & NICHD Pelvic Floor Disorders Network (2018). Effect of Uterosacral Ligament Suspension vs Sacrospinous Ligament Fixation With or Without Perioperative Behavioral Therapy for Pelvic Organ Vaginal Prolapse on Surgical Outcomes and Prolapse Symptoms at 5 Years in the OPTIMAL Randomized Clinical Trial. JAMA , 319 (15), 1554–1565. https://doi.org/10.1001/jama.2018.2827 Weintraub, A. Y., Glinter, H., & Marcus-Braun, N. (2020). Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. International braz j urol : official journal of the Brazilian Society of Urology , 46 (1), 5–14. https://doi.org/10.1590/S1677-5538.IBJU.2018.0581
By Jam Rohr
•
January 20, 2025
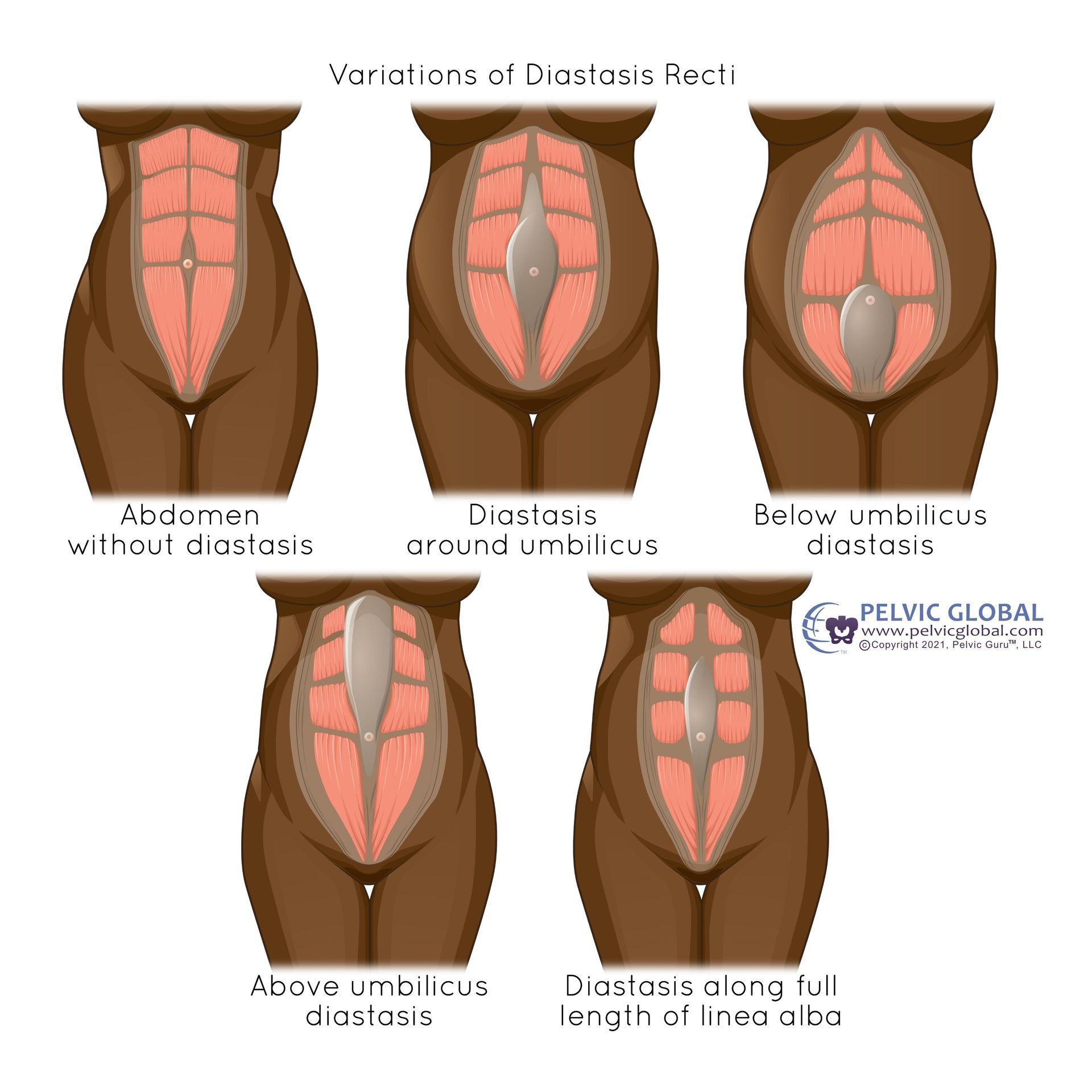
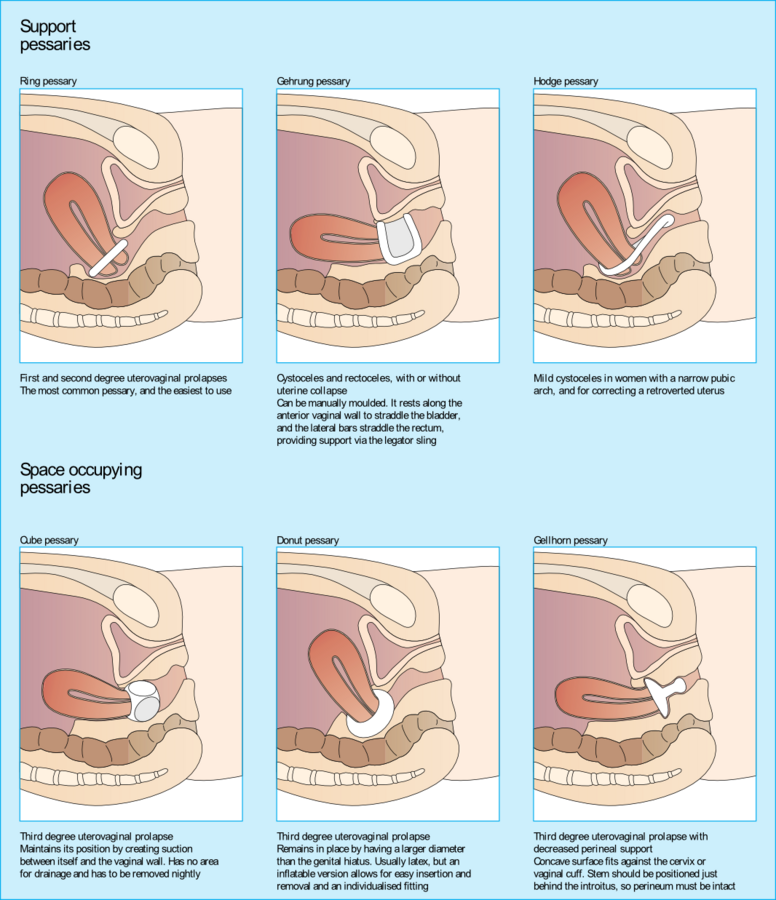
What are Pessaries, and How Do They Work? Pessaries can be awesome, and they can also be really frustrating. But for many people with prolapse, they can be real game-changers! They can improve your symptoms immediately, delay/prevent the need for surgery, and allow you to get back to activities that would normally cause leakage or discomfort. But like any treatment there are upsides and downsides, so let's dive in. What are pessaries? Pessaries are prosthetic devices (like orthotics) that are placed inside the vagina to support the internal organs. They come in MANY shapes and sizes depending upon which organ(s) need(s) support, and what symptoms need improving. They are generally made of silicone but can be made of other medical-grade materials too. My favorite analogy about pessaries is that they are like a sports bra for your internal organs! So there is no shame in needing to use one, especially for higher-impact activities. And just like a sports bra, they don't make the surrounding muscles weaker, they just provide you a little lift right where you need it. Fun fact, pessaries have been around since at least 400 BC. People used to put ALL kinds of things inside vaginas to support the internal organs...my favorite is half a pomegranate soaked in wine as described by Hippocrates! What can pessaries help with? Pessaries help lift organs back toward their original position when they have started to shift due to pelvic organ prolapse. But, pessaries also help control symptoms typically associated with prolapse, like urinary incontinence and pelvic pressure. One of the number one indications for a pessary also is stress urinary incontinence, which most people don't know! So even if you only have stress incontinence with exercise, but don't necessarily have a prolapse, a pessary can still help you. Most of the time we think that pessaries are just helping to decrease symptoms while the pessary is in place. But, there is some emerging evidence to show that regular pessary use can actually improve the grade of the prolapse. This is because the pessary can reduce the strain on the prolapsed organ's ligaments, and then over time those ligaments may shorten and provide better support to the organ. Do they really work? Yes!! Pessaries have a high acceptance rate of over 70% (Vasconcelos 2020). And it's been established in multiple studies that pessaries in combination with pelvic floor muscle training is very effective, more so than either alone (Bugge 2020). Plus, once they are fit well, pessaries generally are a good long-term option. 60% of people are still using their pessaries after 2 years from the initial fitting (Mao 2019). The combo of pessaries and pelvic floor exercises can really make sense when you think about the pressure that a prolapsed organ can place on the pelvic floor. If you always have something pushing down against a muscle you are trying to work, it will be much harder for you to engage/activate that muscle. So, with a pessary in place, your pelvic floor can engage much better and get stronger more easily than without it! Are pessaries helpful for all types of prolapse? Not necessarily - this is the big bummer about pessaries. Pessaries can be incredibly effective for bladder and uterine prolapse. However, for rectoceles (rectum falling into the vagina), pessaries are very hard to fit and much less effective. This is because most pessaries for the bladder and uterus will pop in place by sitting behind the pubic bone. The pubic bone and pelvic floor will act like a little "shelf" to help hold it in place. But, for the backside of the vagina (the rectum), there isn't anything for the pessary to rest against. It doesn't mean that if you have a rectocele you can't find a pessary that works for you, but just remember that it might be a longer and more frustrating process than average. And in the end, you may decide you are better off without a pessary than with one. Who might need a pessary? A pessary can be helpful for you if you: have pelvic organ prolapse have stress incontinence do not need or do not want to have surgery need surgery but are unable to undergo surgery for medical reasons, or because you aren't done having children yet (and yes you can use pessaries while pregnant!) Who may not do well with a pessary? If you fit any of these criteria, a pessary may not be for you: are a smoker have a shortened vaginal length from radiation or any other medical procedures have had prior vaginal surgery have had a pelvic floor avulsion during childbirth (not a typical tear, but where the pelvic floor muscle is pulled off the pubic bone) have fragile vulvar tissues or are otherwise prone to skin breakdown Aren't pessaries just for old ladies? Absolutely not! Anyone can use a pessary at any age and at any stage of prolapse. As we've discussed before, the stage/severity of prolapse and the symptoms of prolapse don't necessarily match. So some people have very minimal prolapse with very severe symptoms, while others can have advanced prolapse with little to no symptoms. So, especially if you've already worked on your pelvic floor, go to PT, etc etc ,and are still struggling with prolapse and/or stress incontinence symptoms, a pessary may be really helpful for you. The bonus to being younger and using a pessary is that it typically means you’ll have an easier time inserting and removing the pessary on your own. Some older people, or generally people with arthritis or limited mobility, can’t reach their vagina well. Or, they may have trouble with the finger dexterity needed to put the pessary in or take it out. So if you don’t live with arthritis or limited mobility and only have symptoms with exercise, you can put the pessary in for exercise and take it out when you are done. Or you can remove it for intercourse and put it back in afterward without a big hassle. And some pessaries you can even leave in for intercourse depending upon their shape and size. How do I insert them, and what do they feel like? Pessaries are really similar to menstrual cups and discs in this manner as most of them are very flexible. You typically squeeze them between your fingers, slide them in vertically, and then they pop into place behind the pubic bone. Once they are inserted, you shouldn't feel them. Other types of pessaries that are called "space-filling" pessaries (like cube pessaries) rely on suction to stay in place. These do not compress in your hand. So those you push up into the vaginal canal like a tampon, and then they will stay in place on their own. What about cleaning? This is a great question and you may get different advice depending upon your sources! The difference here really relies upon whether or not you can insert and remove your pessary on your own. If you are able to do so, then it's recommended you take it out and clean it with soap and water about 1-2x/week. However, I've also heard the argument that if you are only doing it 1-2x/week you are likely to forget! So every day may be best. And if you do have sex with it in, you need to take it out and clean it afterward. If you cannot remove it on your own (especially if you have arthritis in your hands, or otherwise have some limitation with upper extremity mobility), then you do need to visit your doctor once every 3 months to have it removed, cleaned, and re-inserted. Where and how do I get a pessary? Most gynecologists (GYNs) have the ability to fit pessaries. However, depending upon their individual experience they may not feel comfortable fitting all types of pessaries, or may not have a lot of options for you to choose from. So, as I've said in previous posts you may want to see a urogynecologist if you have trouble fitting your pessary, or don't do well with the one your GYN gave you. The good news is that PTs can now fit pessaries too! However, this is very new to the PT scope of practice (at least in the US), so not many PTs are offering this service yet. But if you think about it, it makes sense for PTs to fit pessaries. We have the luxury of spending more time with patients, so we can make sure to get the exact right fit. Plus since we have more space we can usually have you stand up, walk around, even jump or run, etc to make sure it stays in and is comfortable. And we already have experience with things like foot orthotics, so this is just like a foot orthotic for your vagina! I'm excited to see more and more PTs be able to offer this service to their patients. Most of the time pessaries are covered by insurance, but like most things in women's health care, this can be variable. So if you have questions about coverage, make sure to discuss it with your provider, or even better call your insurance company ahead of time. Bottom line Pessaries often get a bad rap or are not thought of for most of us who are younger with prolapse and/or incontinence. But they can be SO helpful, and really should be the first line intervention after pelvic floor exercise/PT for prolapse and stress incontinence! They are pretty cost-effective (certainly less than surgery and PT), don't limit your future options (unlike surgery), and can always be removed and/or changed in size if they become uncomfortable. In fact, it's pretty normal to have to change sizes over time if you use a pessary long-term. Want even more info? Check out some great handouts on pessaries by different urogynecological professional organizations here and here . References: Bugge, C., Adams, E. J., Gopinath, D., Stewart, F., Dembinsky, M., Sobiesuo, P., & Kearney, R. (2020). Pessaries (mechanical devices) for managing pelvic organ prolapse in women. The Cochrane database of systematic reviews , 11 (11), CD004010. https://doi.org/10.1002/14651858.CD004010.pub4 Mao, M., Ai, F., Kang, J., Zhang, Y., Liang, S., Zhou, Y., & Zhu, L. (2019). Successful long-term use of Gellhorn pessary and the effect on symptoms and quality of life in women with symptomatic pelvic organ prolapse. Menopause (New York, N.Y.) , 26 (2), 145–151. https://doi.org/10.1097/GME.0000000000001197 Vasconcelos C, Gomez M, Geoffrian R ,et al. Pessary evaluation for genital prolapse treatment: From acceptance to successful fitting. Neurourology and Urodynamics. 2020;39:2344–2352.

By Jam Rohr
•
January 20, 2025
What are the Best Exercises for Prolapse? There are a LOT of recommendations out there - “do this one exercise to fix your prolapse!” Or, “NEVER do this exercise!” It can be confusing, and frankly overwhelming. So now we are going to take a deep dive to try to answer these questions: what exercises are safe for prolapse, or what are the best exercises to manage prolapse? And, probably the most common question: what should I AVOID if I have prolapse? Pelvic floor muscle training is where it's at I spent a lot of time last article talking about the importance of managing intra-abdominal pressure (IAP). Prolapse is truly more of a top-down issue than a bottom-up one! But after you are better at managing your IAP and not holding your breath, then the first-line intervention always recommended in the literature is pelvic floor muscle training. Notice I keep saying "pelvic floor muscle training," NOT just Kegels. There isn't anything wrong with Kegels, but hopefully, as a Pelvic Love patient, you know that working your pelvic floor goes well beyond just Kegels! We want the pelvic floor to be dynamic and responsive like a trampoline, not hard and stiff like concrete. So working on both strengthening AND relaxing the pelvic floor, longer holds AND quicker flicks, applying pelvic floor muscle activation to exercise AND daily tasks, etc. is all important! Here are some of the benefits of pelvic floor muscle training when you have a prolapse: improvement prolapse symptoms (pressure, heaviness, etc) especially in those with mild to moderate prolapse in prolapse grades 1-3, reduction of the grade of the prolapse reduction of the long-term risk of hospital-based treatment for prolapse (i.e. surgery) How much pelvic floor muscle training is enough? This is the million-dollar question, right? Fortunately for prolapse in particular, we do have some decent evidence on how long it takes to see changes with pelvic floor muscle training. 2 weeks is enough to start to notice a change in symptoms 6 weeks will show a more marked improvement in symptoms 16 weeks may be needed to show improved pelvic floor muscle bulk 6 months may be required before a change in the grade of prolapse is seen After 6 months, the frequency of exercise can be decreased to maintain strength gains, or you can just incorporate the pelvic floor into other exercises Are there specific recommendations for pelvic floor muscle training? In a word (or two :), not really. There isn't enough evidence to say how many sets and repetitions of pelvic floor exercises you need to do. But there are some general guidelines to follow, like: work on your pelvic floor in multiple positions: laying, sitting, standing, squatting, etc choose at least 2-5 days/week to focus on pelvic floor exercises do this for at least 16 weeks And then, don't forget about your core as well! Core stabilization, when added to a regimen including pelvic floor muscle training, can also improve prolapse symptoms. So this basically means, don't forget to incorporate abdominals, multifidus (lower back muscles), breathing, etc. while also working on your pelvic floor! This is basically everything we already do at Pelvic Love Physiotherapy and Wellness! What about different positions just to get some relief from the prolapse symptoms? Many people with prolapse will find that laying in a position with the pelvis elevated, or even doing exercises in this position, is really helpful. Basically by elevating the pelvis you are using gravity to help reduce your organs back to their original position. And then, with the organs not putting so much pressure on your pelvic floor, you will have an easier time activating your pelvic floor too! So some of these positions can include: laying on your back with your bottom elevated on pillows or a wedge (basically a supported bridge) bridges laying down with legs propped on a chair or up the wall (this doesn't technically elevate your pelvis, but can relieve some pressure on the pelvic floor) So what should I NOT do if I have prolapse? As with almost all questions similar to this (such as: what exercises are bad for DR?), it's more about HOW you are doing the exercise vs. WHAT you are doing. And of course, it depends. It depends upon the grade of prolapse, it depends upon how much control you have of your pelvic floor (or not), it depends upon how bad your symptoms are, etc. If prolapse is a new diagnosis for you, we do recommend you avoid impact exercises until you have good control of your pelvic floor, and you know that impact won't exacerbate your symptoms. But once your pelvic floor is strong and still responsive, you have your breathing and abdominals coordinated well with all exercises across all positions, and your symptoms are minimal - you can go back to doing just about anything you want! People have even successfully gone back to higher-level weight lifting, running marathons, etc. with prolapse. The key is managing that intra-abdominal pressure that I talked about last week, and keeping up your pelvic floor strength. Once you have a handle on your IAP and your pelvic floor is working well, the world is your oyster. Sometimes to return to higher-level activities, you may need a little extra help for your prolapse, such as wearing a pessary. It can be inserted for exercise and then removed when you are finished (if you choose not to wear it all of the time). And pessaries are exactly the topic we cover in the next article! So definitely check that one out. References: Fenocchi, L., Best, C., Mason, H., Elders, A., Hagen, S., & Maxwell, M. (2023). Long-term effects and costs of pelvic floor muscle training for prolapse: trial follow-up record-linkage study. International urogynecology journal , 34 (1), 239–246. https://doi.org/10.1007/s00192-022-05272-9 Kashyap, R., Jain, V., & Singh, A. (2013). Comparative effect of 2 packages of pelvic floor muscle training on the clinical course of stage I-III pelvic organ prolapse. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics , 121 (1), 69–73. https://doi.org/10.1016/j.ijgo.2012.11.012 Özengin, N., Ün Yıldırım, N., & Duran, B. (2015). A comparison between stabilization exercises and pelvic floor muscle training in women with pelvic organ prolapse. Turkish journal of obstetrics and gynecology , 12 (1), 11–17. https://doi.org/10.4274/tjod.74317 Wang, T., Wen, Z., & Li, M. (2022). The effect of pelvic floor muscle training for women with pelvic organ prolapse: a meta-analysis. International urogynecology journal , 33 (7), 1789–1801. https://doi.org/10.1007/s00192-022-05139-z
By Jam Rohr
•
January 20, 2025
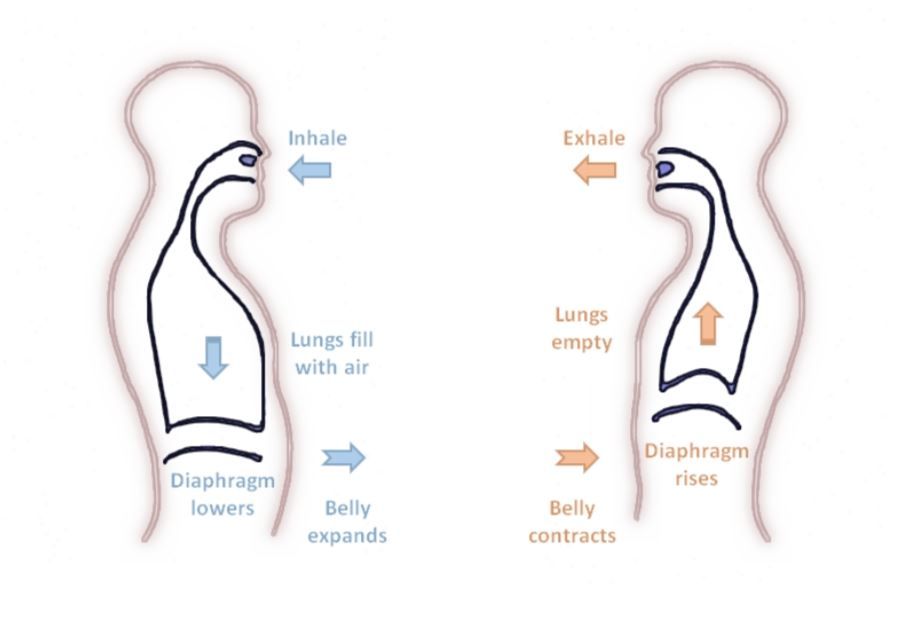
What Does Intra-Abdominal Pressure Have to Do With Prolapse? So far in this series of articles we’ve spent a lot of time talking about what prolapse is exactly, who gets it, and why. It is definitely true that the underlying issue for pelvic organ prolapse is weakness of the connective tissues that help hold up your internal organs, and many of those things are out of your control. But of the things that ARE in your control, they all come down to the same variable: intra-abdominal pressure (IAP) ! What is IAP? IAP is the increased pressure that we create inside our abdomen during physical tasks that either helps push things up and out our nose/mouth (sneezing, coughing, laughing, etc) or down and out your rear end (bowel movements and passing gas). IAP is a necessary part of life; we use increased IAP to our benefit anytime we sneeze or blow our nose, have a bowel movement, cough or laugh, etc. So, I want to be clear that all IAP is NOT bad, as you need it for everyday tasks! The problem becomes when people are increasing IAP as a substitution for lack of core strength, to give them extra “oomph” when lifting or carrying heavy things, or to help put more pressure on their bowels to eliminate their stool if they are constipated. As you can imagine, if you are chronically increasing the pressure inside your abdomen when you really shouldn’t be, this can definitely cause or contribute to your internal organs being pushed out of position. In order to talk about when increasing IAP is and isn’t helpful, we’ll need to do a quick review of breathing mechanics. Your pelvic floor and internal organs SHOULD move With every breath you take, your body does an awesome and intricate dance between your diaphragm, abdominals, and pelvic floor. As you inhale, your diaphragm pushes downwards in order to help fill your lungs with air. This creates increased IAP, which then pushes the belly slightly outwards, and the internal organs and pelvic floor slightly downwards. Then as you exhale, the diaphragm relaxes and elevates as you expel air from your lungs. In turn, this helps pull the pelvic floor and internal organs upwards, and helps the abdominals relax or fall back towards your center. If you want to see this movement in action check out this breathing gif or this abdominal and pelvic floor movement gif . This amazing coordination happens with every. single. breath. that you take! So hopefully this should help illustrate why we always coordinate brace/blink/rocket on the exhale. Coordinating your belly and pelvic floor with the exhale helps keep your IAP low, and naturally helps your body activate your abs and pelvic floor. You can also imagine why prolapse is linked to chronic lung conditions like asthma and COPD, or why you may have worsened prolapse (or incontinence!) with an illness that causes excessive coughing/sneezing. This is also why we don’t want people to get in the habit of holding their breath while exercising or engaging in everyday activities. And it’s also why we don’t want someone to ONLY focus on engaging/strengthening their pelvic floor, and never focus on relaxing it. Your diaphragm gets rigid when you hold your breath, and thus puts a lot of pressure on your internal organs below (illustrated in the second pic). It also doesn’t allow you to properly engage your abs or pelvic floor. The same goes for an overactive pelvic floor - too much rigidity in the pelvic floor doesn’t allow for the natural movement your diaphragm and abdominals should have while breathing, and can cause you to take shorter, shallower breaths. This tension may create more tension in your pelvic organs & fascia, contributing to their descent. In this, and in most cases, motion is lotion! How do I prevent IAP from becoming a problem? In a word, EXHALE! When you exhale fully your IAP is at its lowest. This is due to the natural coordination between your pelvic floor, diaphragm, and abdominals as mentioned above. When the diaphragm elevates and empties your lungs fully of air, it encourages the pelvic floor and abdominals to draw inwards. This provides better support for your internal organs too. This doesn’t mean that it’s always terrible to hold your breath, or you should be scared of taking a deep inhale that causes your belly to bulge a bit and pelvic floor to push downwards/outwards. As explained above, your pelvic floor and internal organs NEED to move. The fear that some people develop after a prolapse diagnosis that prevents them from never fully relaxing their abs and pelvic floor is just as bad as someone who never engages them. Life is all about balance! So, get into the habit of exhaling with any tasks that might increase IAP. This would include lifting anything heavy (from that big bag of dog food to your 20lb infant plus car seat), pushing/pulling anything heavy (heavy grocery carts, moving furniture, etc), light weight-lifting, etc. A special note here for moderate to heavy weights - sometimes this does require you to INCREASE your IAP in able to lift weights safely. If this applies to you, please make sure to work with a personal trainer or other certified fitness professional who can teach you safe techniques for heavier weight lifting. What about deep abs and pelvic floor? Yes, it’s even better if you can coordinate your deep abs (belly brace) and pelvic floor (Kegel) with the exhale during these everyday life tasks! But, the good news is there is a "cheat" if that’s too hard to coordinate (looking at you, the mom with 3 under 5 who has two toddlers asking her 5 million questions while she's lifting the baby out of the car). If you can at least coordinate the exhale during moments of increased IAP, the rest of your muscles will follow. The main point here is that you do not hold your breath with any of these activities. It is also true that some people with prolapse will have INCREASED tension in their pelvic floors, not decreased tension. If you know that is you, then you can ease up on the blink/rocket with increased IAP. But, doing the brace would still be helpful! Next article we’ll dive more into exercises for prolapse, so be sure to check that one out! Reference: Talasz, H., Kremser, C., Talasz, H. J., Kofler, M., & Rudisch, A. (2022). Breathing, (S)Training and the Pelvic Floor-A Basic Concept. Healthcare (Basel, Switzerland), 10(6), 1035. https://doi.org/10.3390/healthcare10061035

By Jam Rohr
•
January 20, 2025
Who Gets Prolapse, and Why? Please note: this post has a brief mention of body weight and obesity. The prevalence of pelvic organ prolapse is one of my favorite things to talk about. Prolapse is SO common, and not enough people know that! Here are some statistics associated with the risk of prolapse (Weintraub 2020): 3-50% of people with vulvas have prolapse 50% of people with vulvas who have been pregnant have prolapse, as do 50% of menopausal people Prolapse increases with age, but prolapse can even be seen in people in their 20s These statistics illustrate why it can get confusing when discussing prolapse because different studies define it differently. The biggest difference between the studies is whether or not the participant has symptoms. Is the study looking at people with symptoms of prolapse like pelvic pressure/heaviness, or difficulty emptying bladder or bowels? Or is the study relying upon an actual diagnosis by a medical professional from completing a vaginal examination? The prevalence of prolapse that does NOT cause symptoms is much higher than that of prolapse that causes symptoms. Some studies will show prolapse occurs in only 3-10% of people with vulvas who have symptoms (ACOG & Abrams), while others show a 94% rate of prolapse if you are talking about grade 1 prolapses that do not cause any symptoms at all (Braekken 2015). In fact, I want to highlight a joint statement by the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS): “Mild descent of the pelvic organs is common and should not be considered pathologic. Pelvic organ prolapse should only be considered a problem if it is causing prolapse symptoms (ie, pressure with or without a bulge) or sexual dysfunction or if it is disrupting normal lower urinary tract or bowel function.” So, if you have a mild prolapse especially (grade 1), try not to get too worried! If you need a review on the grades or prolapse, please check out my article Prolapse is Confusing! What Types of Prolapse are Most Common? This is also where the literature is really interesting, and shows more truths that are not discussed often. In people who are diagnosed with prolapse, these are the rates of the different types of prolapse seen: (Abrams 2017) Cystocele (bladder) 16-25% Rectum (rectocele) 13-19% Uterus 5-14% And of those, the vast majority have grades 1 or 2 prolapse. But guess what….. 65% of people with prolapse have some grade of prolapse of all 3 organs. That’s right - unfortunately, when one organ starts to fall, the rest tend to come with it. This is especially true of the uterus. The uterus and cervix are kind of like the roof of the house of your vagina. And once the roof starts to fall in, it tends to take the walls with it. What About Postpartum Prolapse? This is also incredibly common, and again not discussed often. Durnea 2014 found these rates in a smaller study of 202 people with vulvas who were one year postpartum after their FIRST baby: 89% had uterine prolapse 90% had cystocele 70% had rectocele And again, the majority of these study participants had prolapse in multiple compartments. Plus, 80% had no symptoms as the majority of these were grades 1 and 2. And, the majority of these participants also were young - 78% were under the age of 34. The study didn’t do any long-term follow-up, so my suspicion is that these conditions likely improved over time as the demands of childcare were less, and the participants returned to their pre-partum levels of strength and activity. What Are the Risk Factors for Prolapse? This is another one I love to talk about, because it helps to realize that developing prolapse is largely out of an individual person’s control. The main “cause” of prolapse is a weakening of the fascia and ligaments that help hold up your internal organs. Your pelvic floor strength, or lack thereof, can contribute to prolapse, but typically is not the primary problem. Here is a non-exhaustive list of risk factors: Having a vagina is number one (a larger space in the pelvis required for childbirth also means more space for organs to change position) Being pregnant, especially more than once (parity) Vaginal childbirth, especially pushing more than 2-3 hours or the need for forceps/vacuum Genetics/family history Connective tissue disorders (joint hypermobility) Menopause specifically, as well as simply aging Pelvic trauma/injury Heavy lifting Chronic constipation/straining Lung disorders or chronic coughing Poor nutrition Smoking Higher body weight/mass due to pressure placed on the internal organs (please note: in the graphic it does say “obesity,” which is not our choice of words) Race/ethnicity Hysterectomy Hopefully this helps pull back the curtain a bit on why you may have prolapse (if you do), and help you realize that it’s not your fault. Make sure to check out the next article that discusses intra-abdominal pressure, which is really the link behind all of these issues, and is the key to avoiding making your prolapse worse! References: Abrams,P, Cardozo, L, Wagg, A, Wein, A. (Eds) Incontinence 6th Edition (2017). ICI-ICS. International Continence Society, Bristol UK, ISBN: 978-0956960733. American College of Obstetricians and Gynecologists and the American Urogynecologic Society, & INTERIM UPDATE: This Practice Bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. (2019). Pelvic Organ Prolapse. Female pelvic medicine & reconstructive surgery , 25 (6), 397–408. https://doi.org/10.1097/SPV.0000000000000794 Braekken, I. H., Majida, M., Ellström Engh, M., & Bø, K. (2015). Can pelvic floor muscle training improve sexual function in women with pelvic organ prolapse? A randomized controlled trial. The journal of sexual medicine , 12 (2), 470–480. https://doi.org/10.1111/jsm.12746 Durnea, C. M., Khashan, A. S., Kenny, L. C., Durnea, U. A., Smyth, M. M., & O'Reilly, B. A. (2014). Prevalence, etiology and risk factors of pelvic organ prolapse in premenopausal primiparous women. International urogynecology journal , 25 (11), 1463–1470. https://doi.org/10.1007/s00192-014-2382-1 Weintraub, A. Y., Glinter, H., & Marcus-Braun, N. (2020). Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. International braz j urol : official journal of the Brazilian Society of Urology , 46 (1), 5–14. https://doi.org/10.1590/S1677-5538.IBJU.2018.0581
By Jam Rohr
•
January 20, 2025
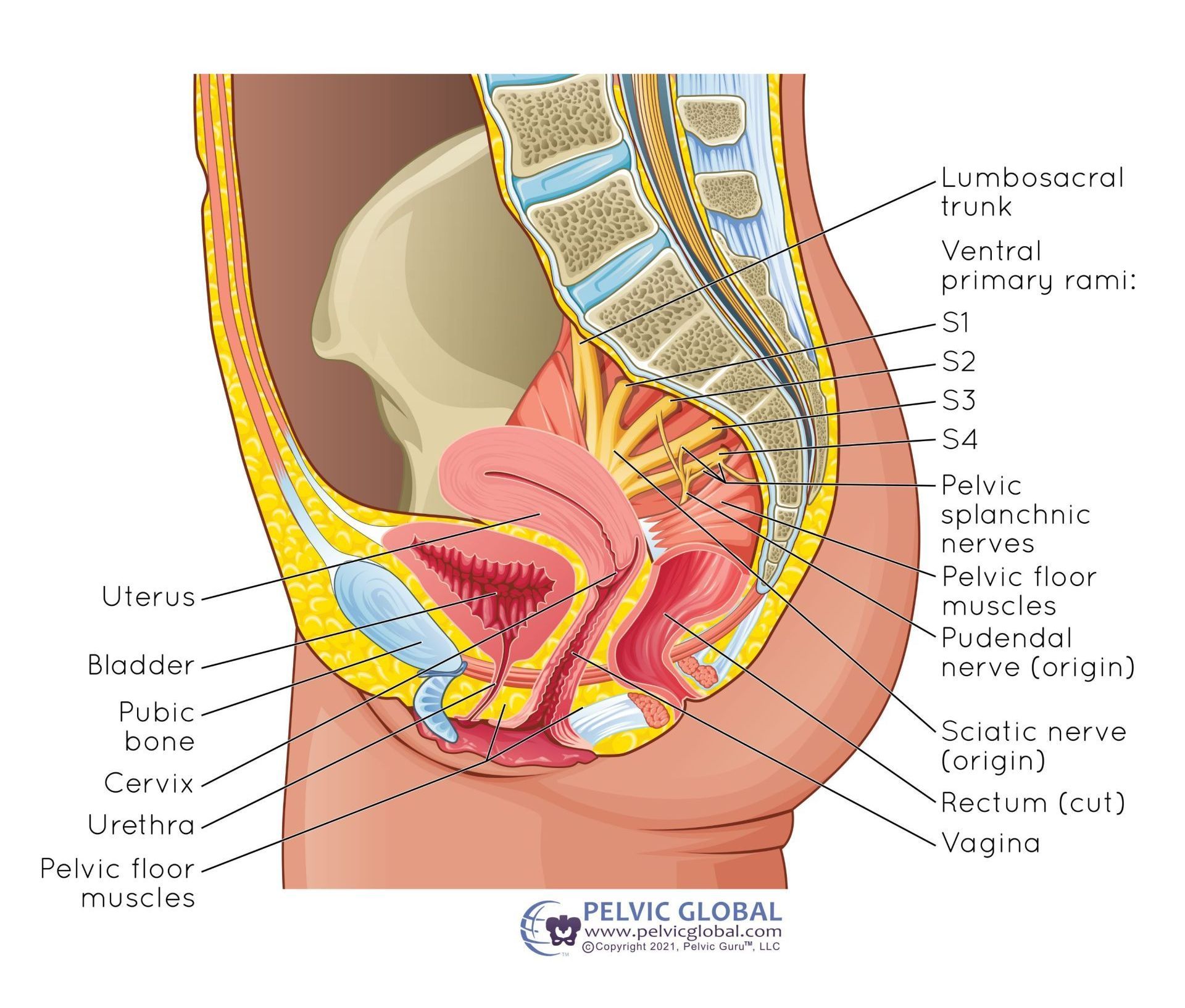
Prolapse is Confusing! If you've been diagnosed with, or ever suspected that you have, pelvic organ prolapse, I'm certain it brings up a million questions for you. Will my bladder eventually fall out of my vagina? Will having sex make it worse? Do I need surgery? What about having more kids, returning to exercise and running, etc etc?? These are all FANTASTIC questions that typically don't get explained very well by the person who diagnoses you with prolapse, or by doing your own internet research. And, most of these difficulties originate with the fact that prolapse is not just one diagnosis. There are so many different organs that can prolapse, and so many different grades of prolapse, that it can be incredibly confusing. So today, let's start with the basics: what is prolapse, and how do we diagnose and grade it? What is Prolapse? The definition of prolapse is when "an organ or organs in the pelvic cavity shift downward out of their normal position." (Palm 2017) What are the Types of Prolapse? Vaginal prolapse can occur from the bladder (cystocele), the rectum (rectocele), the uterus/cervix (apical or uterine prolapse), the small intestines (enterocele), or the vaginal vault (vaginal vault prolapse only happens in individuals who have had a total hysterectomy). It's also important to note that similar to a hernia, the “bulge” created by a prolapse is the organ pushing the vaginal wall downwards or outwards. As a result, the tissue you are actually seeing or feeling is the vaginal wall, not the organ itself. So no, your bladder or bowel will not just fall out one day! The only exception to this is cervical/uterine prolapse, where you will actually feel or see the cervix if it gets low enough. But, I promise that still won’t fall out one day either! You can also have prolapse outside of the vaginal canal - the urethra can descend from its original position towards the vulva (urethrocele), or the lining of the rectum can prolapse outside of the anus (rectal prolapse). {NOTE: this is why language is important; many people will talk about a "rectal prolapse" when they really mean a rectocele. Rectal prolapse external to the anus requires surgical correction - no amount of pelvic floor exercises will help.} WHEW that's a lot. So, before you freak out and worry about just exactly how many of your organs will eventually fall out of your vagina (haha), let's talk about grading and statistics! How do we Grade Prolapse? This is super important. - not all prolapses are created equal! There is a VERY big difference between minor prolapses (the bladder just slightly bulging into the vagina) vs major prolapses (the cervix or uterus being external to the vagina). There are a few different grading scales out there, but here are the most common grades: Prolapse is less than halfway to the opening of the vagina Prolapse is more than halfway to, or AT the opening of the vagina Prolapse is EXTERNAL TO the opening of the vagina Maximal descent of the entire organ outside of the vagina The good news is that prolapse is a slowly progressing condition. So no, you won't go from a grade 1 to a grade 3 overnight. Grade 4 students are rare, especially in higher-income countries. Typically it takes years for prolapse to worsen, if it does worsen at all. In upcoming posts we'll talk about what does and doesn't cause prolapse, and if you do have prolapse what you can do to help it get better (or at least not get worse). Who Can Diagnose Me with Prolapse? This is also an excellent question with a very nuanced answer. Your gynecologist (GYN) can do so, but the prolapse specialists are truly urogynecologists (urogyns) or in some cases colorectal surgeons, particularly for rectoceles. A pelvic floor PT can also diagnose you with prolapse, but we can't say with certainty which organ is prolapsing - we typically talk more about which wall of the vaginal canal is bulging. A pelvic floor PT also typically can do a more detailed assessment than your GYN, as we also can assess people in standing positions. Sometimes prolapses are tricky to see when you are laying flat on your back, so a standing examination can be very useful! If someone is concerned about their prolapse diagnosis, I do typically recommend they seek a consultation with a urogynecologist. This usually occurs when they have been told they don't have a prolapse when they think they do, or have been blindsided with a diagnosis of higher-degree or multiple-organ prolapse when they were unaware. A urogyn can do a much more detailed assessment of prolapse than a GYN can, and they are also experts at fitting pessaries or performing corrective surgeries. More on this in upcoming posts! But if you are curious, you can look up a urogyn close to you or a colorectalsurgeon (for rectoceles or rectal prolapse). I will say also that typically fancy imaging studies are not needed to diagnose prolapse. They can be used in certain cases, for example, if you have constipation and a rectocele, there is a special test that can be done to see how much of your rectum is falling into the vagina when you are bearing down to pass stool. But, this is definitely the exception rather than the rule. Usually, the examination done in the office is all that is needed. What Else Should I Know About Pelvic Organ Prolapse? Voices for Pelvic Floor Dysfunction Association for Pelvic Organ Prolapse Support International Urogynecological Association patient information leaflets American Urogynecological Association patient fact sheets Reference: Palm, S. (2017). Pelvic Organ Prolapse: The Silent Epidemic (3rd ed.). POP Publishing and Distribution.
© 2025
All Rights Reserved | Pelvic Love Physiotherapy & Wellness, PLLC